A SHORT HISTORY OF B-Cell HLA EPITOPES
written by Ilias Doxiadis; Henry Loeffler-Wirth; Nils Lachmann; Claudia Lehmann
https://doi.org/10.1159/000538447
ABSTRACT
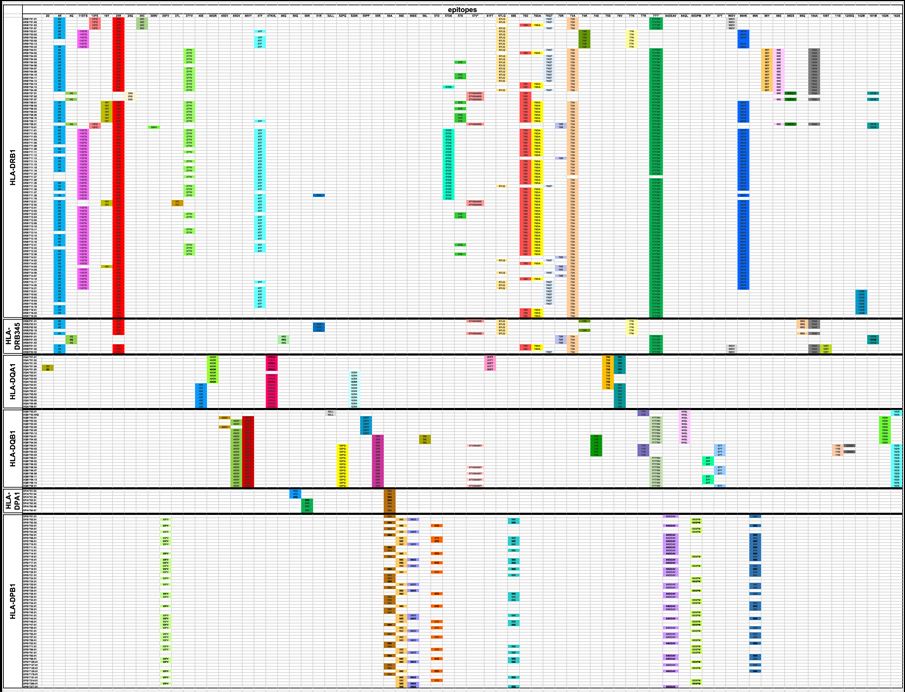
Background: HLA epitopes are currently in the focus of transplantation immunogenetics. The main reason is the complexity of the HLA system with >38,000 alleles, the number of which increases steadily. These alleles are determined by the current state-of-the art typing methods like second- and third-generation sequencing. Screening for HLA antibodies is hampered by the lack of specific target beads with all possible alleles described. Summary: A way to circumvent the problem is to define HLA epitopes. The number of antibody-confirmed epitopes, on the other hand, was found to be 72 for HLA class I and 74 for HLA class II. Here, we elaborate on the current knowledge on these HLA epitopes. Absolute definitions of these structures are not yet available. Key Messages: Making use of eplets is a comparable way allowing statistical analyses. However, one should keep in mind that the results obtained are approximative or perhaps better associative. Continuous collaboration is needed for the full understanding of the HLA epitopes. The reactivity toward epitopes remains patient-specific.
INTRODUCTION
Antibodies recognize a partial subregion of an antigen, which is termed epitope. Consequently, only a few amino acids of the antigen are “seen” and hence determine the specificity. The surrounding amino acids interact with the stabilization of the antigen-antibody complex. These few amino acids although specific are in many of the cases found on several HLA class I or II molecules. Consequently, HLA antibodies interact with numerous HLA molecules and not a single molecule [1, 2].
. . .
CONCLUSION
Defining HLA epitopes circumvents the problems of the ever increase in numbers of the HLA alleles worldwide. They can be used for a variety of purposes, especially for organ and stem cell transplantation since the latter is steadily using HLA mismatched donors. The accurate definition of these epitopes will soon allow better predictions with respect to their influence on patient and graft survival. However, one should keep in mind the individuality of the patient (solid organ) or donor (stem cell): Although several authors show a statistical effect of the total number of epitope mismatches in the context of transplantation [34, 35], the important role is the individual epitope which acts for the patient as the immunogen, as Dankers et al. [36] and Doxiadis et al. [37] reported earlier. This individuality of the patients might explain the differences in the results when different populations are analyzed. For the future, organ allocation organization should aim in the definition of donor-specific epitopes for the population they serve. These values would be used instead of the currently used v-PRA [38] or c-PRA [39].
In our opinion, prior to making statements on the immunogenicity of epitopes, the frequency of the epitope in the tested population (epiPRA %) should be considered and for which patient phenotypes the epitope is prone to antibody production. With state-of-the-art HLA typing methods and a more advanced understanding of epitopes, a much more individualized organ allocation would be possible in the future.
countable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved and gave the final approval of the version to publish.
to read the full article, click here: https://karger.com/tmh/article/doi/10.1159/000538447/906205/A-Short-History-of-B-Cell-HLA-Epitopes